A closer look at how machine intelligence is helping doctors see cancer in an entirely new light.
Updated
January 8, 2026 6:33 PM

Serratia marcescens colonies on BTB agar medium. PHOTO: UNSPLASH
Artificial intelligence is beginning to change how scientists understand cancer at the cellular level. In a new collaboration, Bio-Techne Corporation, a global life sciences tools provider, and Nucleai, an AI company specializing in spatial biology for precision medicine, have unveiled data from the SECOMBIT clinical trial that could reshape how doctors predict cancer treatment outcomes. The results, presented at the Society for Immunotherapy of Cancer (SITC) 2025 Annual Meeting, highlight how AI-powered analysis of tumor environments can reveal which patients are more likely to benefit from specific therapies.
Led in collaboration with Professor Paolo Ascierto of the University of Napoli Federico II and Istituto Nazionale Tumori IRCCS Fondazione Pascale, the study explores how spatial biology — the science of mapping where and how cells interact within tissue — can uncover subtle immune behaviors linked to survival in melanoma patients.
Using Bio-Techne’s COMET platform and a 28-plex multiplex immunofluorescence panel, researchers analyzed 42 pre-treatment biopsies from patients with metastatic melanoma, an advanced stage of skin cancer. Nucleai’s multimodal AI platform integrated these imaging results with pathology and clinical data to trace patterns of immune cell interactions inside tumors.
The findings revealed that therapy sequencing significantly influences immune activity and patient outcomes. Patients who received targeted therapy followed by immunotherapy showed stronger immune activation, marked by higher levels of PD-L1+ CD8 T-cells and ICOS+ CD4 T-cells. Those who began with immunotherapy benefited most when PD-1+ CD8 T-cells engaged closely with PD-L1+ CD4 T-cells along the tumor’s invasive edge. Meanwhile, in patients alternating between targeted and immune treatments, beneficial antigen-presenting cell (APC) and T-cell interactions appeared near tumor margins, whereas macrophage activity in the outer tumor environment pointed to poorer prognosis.
“This study exemplifies how our innovative spatial imaging and analysis workflow can be applied broadly to clinical research to ultimately transform clinical decision-making in immuno-oncology”, said Matt McManus, President of the Diagnostics and Spatial Biology Segment at Bio-Techne.
The collaboration between the two companies underscores how AI and high-plex imaging together can help decode complex biological systems. As Avi Veidman, CEO of Nucleai, explained, “Our multimodal spatial operating system enables integration of high-plex imaging, data and clinical information to identify predictive biomarkers in clinical settings. This collaboration shows how precision medicine products can become more accurate, explainable and differentiated when powered by high-plex spatial proteomics – not limited by low-plex or H&E data alone”.
Dr. Ascierto described the SECOMBIT trial as “a milestone in demonstrating the possible predictive power of spatial biomarkers in patients enrolled in a clinical study”.
The study’s broader message is clear: understanding where immune cells are and how they interact inside a tumor could become just as important as knowing what they are. As AI continues to map these microscopic landscapes, oncology may move closer to genuinely personalized treatment — one patient, and one immune network, at a time.
Keep Reading
How a Korean biotech startup is using AI to move drug discovery from trial-and-error to precision design
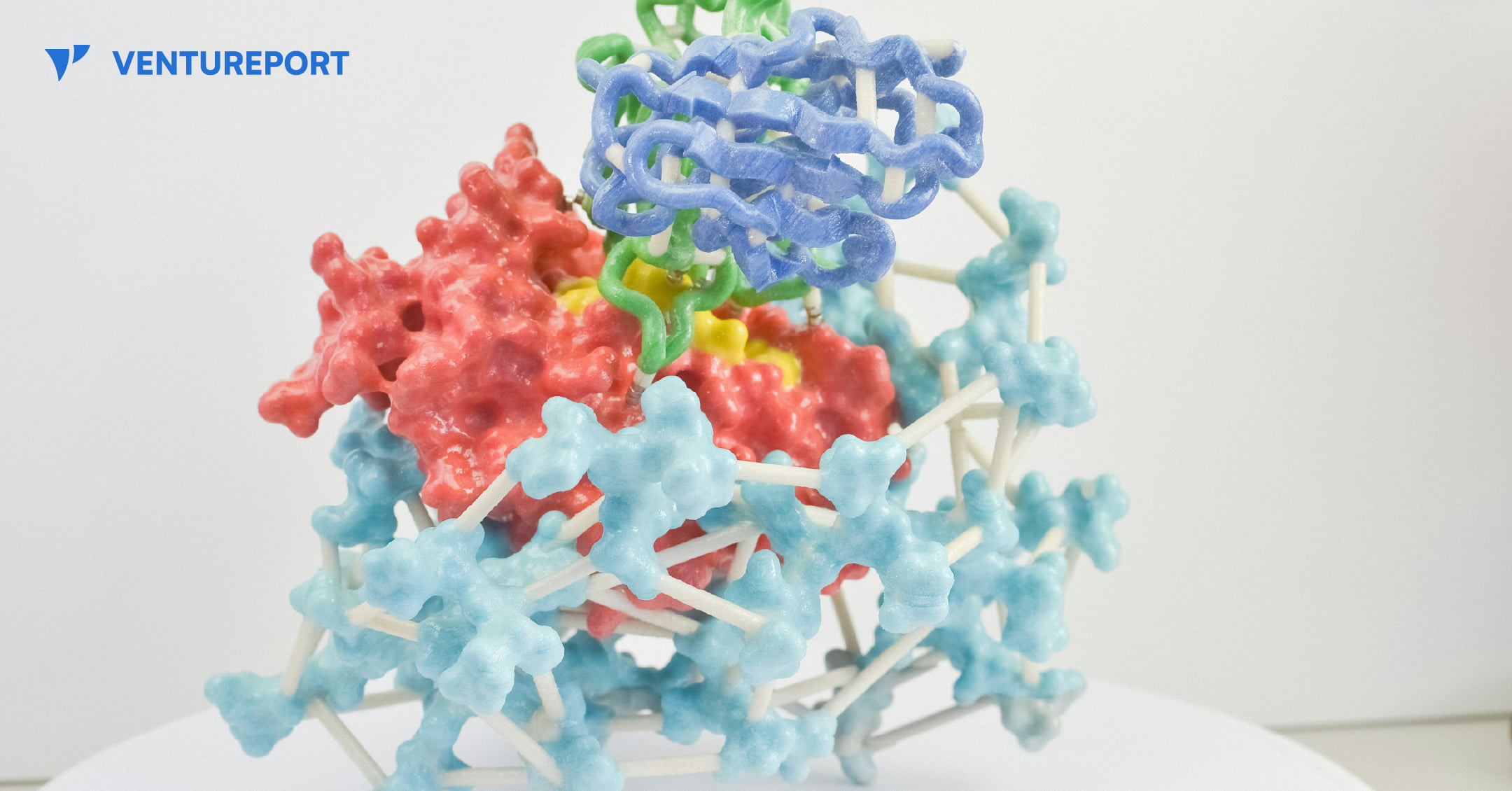
A close up of a protein structure model. PHOTO: UNSPLASH
For decades, drug discovery has relied on trial and error, with scientists testing thousands of molecules to find one that works. Galux, a South Korean biotech startup, is changing that by using AI to design proteins from scratch. This method, called “de novo” design, makes it possible to build precise new therapies instead of searching through existing ones.
The company recently announced a US$29 million Series B funding round, bringing its total capital to US$47 million.This significant investment attracted a substantial roster of institutional backers, including the Korea Development Bank (KDB), Yuanta Investment, SL Investment and NCORE Ventures. These firms joined existing investors such as InterVest, DAYLI Partners and PATHWAY Investment, as well as new participants including SneakPeek Investments, Korea Investment & Securities and Mirae Asset Securities.
At the core of the company’s work is a platform called GaluxDesign. Unlike many AI tools that only predict how existing proteins fold, this system uses deep learning and physics to create entirely new therapeutic antibodies. This “from scratch” approach lets the team go after so-called “undruggable” proteins. These are targets that traditional small-molecule drugs can’t reach because they lack clear binding pockets. By designing proteins to fit these complex shapes, Galux aims to unlock treatments that have stayed out of reach for decades. And that’s exactly why investors are paying attention.
The pharmaceutical industry is actively looking for faster and more efficient ways to develop new drugs, and Galux is built for exactly that. The company connects its AI platform directly to its own wet lab, where designs can be tested in real time. Each result feeds straight back into the system, sharpening the next round of models. This continuous loop speeds up discovery and improves precision at every step. It’s also why partners like Celltrion, LG Chem and Boehringer Ingelheim are already working with Galux.
Galux is no longer just trying to make drugs that stick to a target. The company now wants its AI to design medicines that actually work in the body and can be made at scale. In simple terms, a drug has to do more than bind to a disease—it must be stable, safe and strong enough to change how the illness behaves. Galux is moving into tougher targets such as ion channels and GPCRs. These play key roles in heart function and sensory signals. Ultimately, the goal is to show that AI-driven design can turn complex biology into real treatments. And instead of hunting blindly for a solution, the team is building exactly what they need.